Good news | CDE officially approved the aCGT "Human Umbilical Cord Mesenchymal Stem Cell Injection" to enter clinical trials
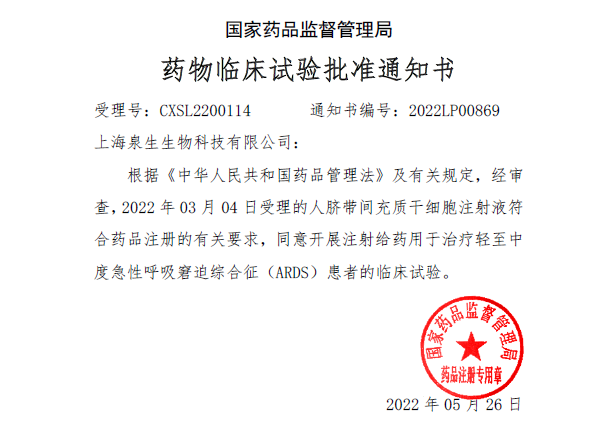
On May 26, 2022, aCGT's independently developed Class I biological drug, "Human Umbilical Cord Mesenchymal Stem Cell Injection" (acceptance number CXSL2200114), officially obtained clinical trial approval from the Drug Evaluation Center (CDE) . Source: Official website of CDE Notice of approval of drug clinical trials by the State Food and Drug Administration The IND approval marks a milestone in the field of stem cell drug research and development, and it is also the world's first new stem cell drug that is expected to be used for acute respiratory distress syndrome (ARDS), which is of great significance to the entire field of stem cell therapy. 1、Learn about acute respiratory distress syndrome 1. Causes of ARDS Acute respiratory distress syndrome (ARDS) refers to the excessive activation of an inflammatory response in the lungs or even throughout the body due to various causative factors. It is characterized by destruction of the pulmonary epithelium and vascular endothelium, decreased alveolar clearance, and diffuse alveolar injury on imaging. Alveolar epithelial injury and pulmonary endothelial injury caused the accumulation of protein-rich inflammatory edema fluid in the alveolar cavity in the pathological samples of the patient. To put it simply, it is the leakage of fluid from the blood vessels into the alveoli, making it difficult for the patient to breathe, or even unable to breathe. There are many factors that cause ARDS, such as sepsis, multiple injuries, massive blood transfusions, aspiration pneumonia, pulmonary contusion and cardiopulmonary bypass, among which sepsis and severe lung infection are the main causes of ARDS in clinical practice. Studies have shown that among the first 41 patients admitted to the hospital in Wuhan, ARDS was the fatal complication with the highest incidence (29%). 2. Pathogenesis of ARDS The pathogenesis of ARDS is complex, and the most recognized mechanism is that various etiologies induce the increase in the production of pro-inflammatory factors in the lungs, and the release and activation of a large number of inflammatory factors make the inflammatory response in the lungs uncontrollable, and the pulmonary capillary endothelial cells and alveolar epithelial cells are damaged, resulting in dysfunction. The release of reactive oxygen species from injured endothelial cells can increase the permeability of lung endothelial cells, and a large amount of protein-rich substances enter the bronchial and alveolar spaces, resulting in pulmonary edema, thereby reducing the efficiency of pulmonary ventilation and even respiratory failure in the body, which is difficult to correct. 3. Traditional treatment modalities for ARDS Currently, treatment for ARDS includes primary disease treatment, protective mechanical ventilation, and pharmacotherapy. Drug therapy for ARDS includes anti-inflammatory drugs (e.g., glucocorticoids), antioxidant therapy (e.g., N-acetylcysteine), and alveolar surfactant replacement therapy. However, neither anti-inflammatory drugs (e.g., corticosteroids, neutrophil elastase inhibitors) nor drugs that attempt to improve the lungs themselves (e.g., inhaled β agonists) are currently unable to effectively reduce the mortality of ARDS, and mechanical ventilation is still the main clinical treatment. However, mechanical ventilation uses a ventilator to control the air pressure to expand the alveoli, which may cause alveolar wall damage and further induce mechanical ventilation-related lung injury. 4. The importance of developing effective drugs for the treatment of ARDS ARDS is a common critical illness in clinical practice, one of the main causes of respiratory failure, and has a high mortality rate in ICU patients. Epidemiological studies show that there are about 3 million ARDS patients in the world every year, and the incidence rate of intensive care unit patients is about 10%, and the mortality rate is 30%~40%. So far, there is still a lack of breakthroughs in the international medical community for the treatment of ARDS, and many drugs that have shown potential in preclinical studies have failed to succeed in clinical trials, and the novel coronavirus pneumonia epidemic has further highlighted the importance of developing effective drugs for the treatment of ARDS. 2、Stem cell therapy for acute respiratory distress syndrome With the advancement of basic research in recent years, the relevant mechanisms of ARDS have been continuously revealed. Due to the complexity of the cause and pathology of this disease, it may be a valuable research direction to carry out targeted multi-means combination therapy according to the actual situation of patients. As a new type of treatment, stem cell therapy has attracted widespread attention, and stem cell therapy has obvious effects in many diseases. For example, liver failure, osteoarthritis, GVHD, cardiovascular and cerebrovascular diseases have become popular research directions in the medical field. Numerous studies have confirmed that mesenchymal stem cells (MSCs) also have a good therapeutic effect in lung injury: 01 MSCs have the functions of differentiation, regeneration and repair Exogenous MSCs can "homing" at the site of injury to induce differentiation into lung tissue cells such as mesenchymal fibroblasts, myofibroblasts, lung epithelial cells, vascular endothelial cells and smooth muscle cells, thereby alleviating lung injury. 02 MSCs have immunomodulatory functions MSCs have an inhibitory effect on the inflammatory response to ARDS overactivation. In addition, MSCs can also inhibit inflammatory levels by secreting a series of anti-inflammatory cytokines, while regulating the function of body systems, enhancing bacterial clearance, reducing bacteremia, and improving pulmonary vascular permeability. 03 MSCs have paracrine effects MSCs secrete a variety of cytokines and active metabolites into the microenvironment to reduce inflammation. For example, IL-6, PGE-2, and IL-10 secreted by MSCs can inhibit T cell proliferation and prevent dendritic cell maturation. Other cytokines and a range of proteoglycan complexes have also been shown to inhibit the inflammatory response of overactivity in damaged areas. MSCs release particulates into the environment. A microparticle is a biologically active small membranous vesicle containing proteins, mRNA, miRNA, and other bioactive substances that can be used as mediators to participate in cell-to-cell "communication" and regulate immune cell behavior. aCGT "Human Umbilical Cord Mesenchymal Stem Cell Injection" can inhibit the inflammatory response of ARDS overactivation, which can safely and effectively solve the "root cause" of the disease, and treat and overcome ARDS from the essence of the disease. In addition, based on the regeneration, repair, immune regulation and paracrine characteristics of stem cells, aCGT "Human Umbilical Cord Mesenchymal Stem Cell Injection" can be used for the treatment of a variety of other major and difficult problems of diseases, including non-specific inflammatory therapy, tissue regeneration, autoimmune diseases, etc., to meet more "unmet clinical needs". The research team of aCGT always adheres to patient-centered benefits, promotes clinical research of stem cell products with high quality, and converts them into trustworthy products. We practice the mission of giving everyone the opportunity to master life.